You have activated the high contrast version of the site. For more info on this topic, please visit this page.
New criteria to avoid the over-diagnosis of Alzheimer’s Disease
Diagnosis of Alzheimer’s Disease (AD) is currently largely based on the presence of biomarkers. This may lead to a problematic over-diagnosis if this is incorrectly interpreted.
To counter this problem, a global expert panel led by Hôpitaux universitaires de Genève (HUG), the University of Geneva and the Salpêtrière Hospital have drawn up recommendations. Based on a review of the scientific literature, they advocate that clinical signs as well as biomarkers must be taken into account. This new approach avoids diagnosing AD in people with abnormal biomarkers who will never develop memory disorders and sets out a monitoring process tailored to each individual. These recommendations have been published in the Journal of the American Medical Association – Neurology (JAMA Neurology).
According to the Association Alzheimer Suisse, by 2050 the number of people in Switzerland affected by AD and other forms of dementia will exceed 300,000, which is twice as many as today.
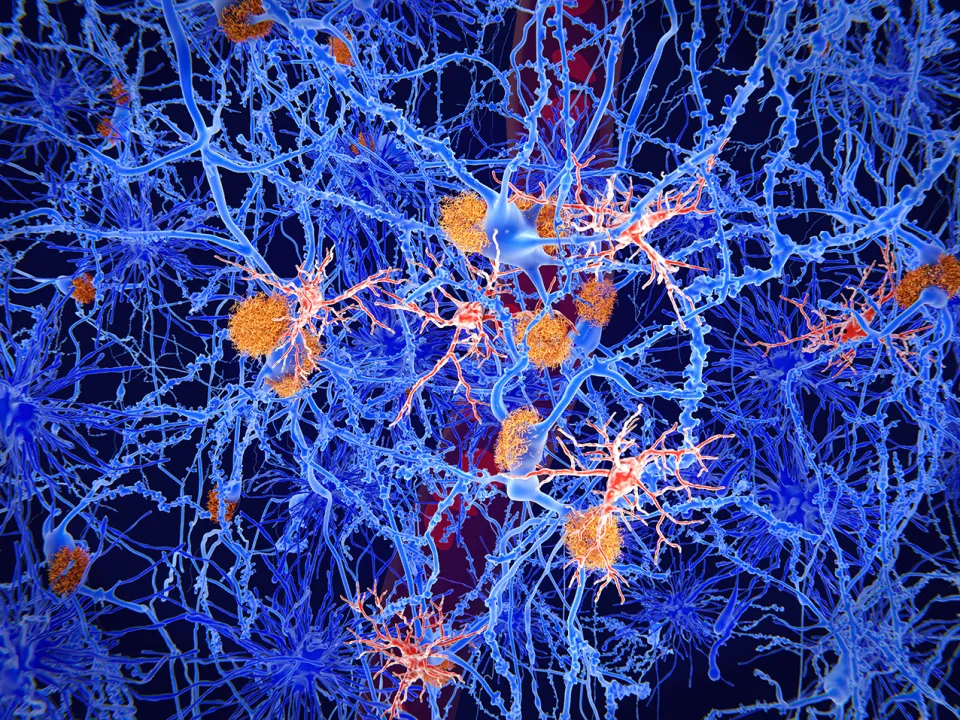
To facilitate research into this disease, three months ago a group of scientists in the United States defined new very broad diagnostic criteria. For them, an AD diagnosis would be defined by the sole presence of biomarkers, such as amyloid β and tau protein, without taking memory function and other cognitive functions into account. These biomarkers are quantifiable in cerebrospinal fluid, on PET brain images or in the blood and have been associated with the cerebral degeneration that gives rise to AD.
For the global expert panel led by Prof. Giovanni Frisoni, Head of the Memory Center at theHUG and Full Professor, Department of Readaptation and Geriatrics at the UNIGE Faculty of Medicine and Professor Bruno Dubois, Professor of Neurology at Sorbonne University and Head of Department at the Salpêtrière Hospita in Parisl, the impact of these new criteria will be that numerous, perfectly healthy people, will be diagnosed with AD on the sole basis of a laboratory examination, whereas they will never develop memory disorders. Therefore, they formed an expert panel to issue new recommendations.
A clinical and biological definition
According to Professors Frisoni, Dubois and their colleagues, biomarkers are only useful if they are associated with a multidisciplinary medical consultation and with memory tests. These tests may reveal short-term memory problems namely the inability to retain recent information.People affected may also lose their points of reference and become disoriented. They will often have difficulty speaking, finding their words or their reasoning will become less clear. Finally, behavioral changes such as irritability, anxieties, depression and social isolation sometimes also occur.
This diagnostic nuance is crucial for individuals who have positive biomarkers but who do not manifest clinical symptoms. If these represent only 3% in the 50 to 59 age range, this figure rises to 40% in the 80 to 89 age range. Based on the criteria of the American Alzheimer's Association, all these people would qualify for an AD diagnosis. However, for Professor Frisoni, “70% of all these people will never develop AD.” Therefore, why give them this distressing diagnosis?”
New categories
The recommendation of the international team comes down to reconsidering biomarkers not as equivalents of AD but simply as indicators of the deposit of toxic proteins that go hand in hand with the disease. This nuance enables two categories of individuals with abnormal biomarkers to be defined, those with abnormal memory tests and those with normal tests. The first group has AD whereas the second group only has an increased risk of developing AD, but does not have it yet. They are therefore not considered to be ill, but rather at risk.
A new patient journey in Geneva
Within the clinical context, these categories allow new monitoring strategies to be developed for people at risk who are not currently being treated. In Geneva, changes in best practice have already been set into motion. “We have received funding from the State of Geneva for four years so that by early 2025 our Memory Center will be able to offer a new patient journey for people at risk. These journeys will also specifically include an evaluation of all known risk factors, including biomarkers, but also depression and social isolation.”
Future research challenges
The formulation of these two categories of individuals is also important for research as they will enable better stratified longitudinal cohorts to be created. “The weight of each risk factor is quite imprecise for the moment, clarifies Professor Frisoni, and the addition of these categories in longitudinal studies will allow us to quantify the weight of each factor much more accurately.” The inclusion of asymptomatic individuals in clinical trials will also allow for testing the effectiveness of treatments, including amyloid lowering agents, seeking to reduce the risk of developing AD and the associated cognitive impairments. “In the long term, we envision personalized treatments based on lifestyle and nutritional principles such as probiotics, as well as on anti-amyloid drugs, tailored to the individual's risk profile”, concludes Prof. Frisoni.
JAMA Neurol. doi:10.1001/jamaneurol.2024.3770
Please also consult our Press Release of 15 February 2024 on the European consensus on AD diagnosis